The Critical Role of Time and Attendance Tracking in Healthcare

Ensuring Excellence in Patient Care through Precision
Accurate time and attendance tracking is indispensable in the healthcare industry, where the stakes are incredibly high. Whether it’s ensuring that a nurse is available when a patient requires immediate attention or making certain that all regulatory requirements are met, the precision of time and attendance systems directly impacts both patient outcomes and operational efficiency. Consider the ramifications of understaffing, which can lead to delayed treatments, or administrative errors that result in hefty non-compliance fines. These scenarios underscore the necessity of robust time and attendance systems to maintain smooth and effective healthcare operations.
Enhancing Efficiency, Compliance, and Patient Care
The advent of modern time and attendance systems has brought significant advancements to the healthcare sector, transforming how facilities manage their operations. These innovative systems facilitate the efficient handling of complex schedules, significantly reduce administrative workloads, and foster a more reliable environment for both healthcare professionals and patients. This blog will explore the extensive benefits these systems offer, the challenges they help overcome, and the best practices for their implementation within healthcare settings. By examining these aspects, we will reveal how the integration of these technologies can lead to a more efficient, compliant, and patient-centric healthcare environment.
‘Pro-Tip’
Implement Biometric Authentication for Accuracy: Use TimeTrex’s biometric authentication features, such as or facial recognition, to ensure accurate and secure time tracking. This prevents “buddy punching” and ensures that only authorized personnel can clock in and out.
Why Time and Attendance Management is Crucial in Healthcare
Direct Impact on Patient Care
Efficient time and attendance management directly influences the quality of patient care in healthcare facilities. When staff members’ attendance is accurately tracked, it ensures that the right number of healthcare professionals are available to meet patient needs at all times. This precision is vital in avoiding understaffing or overstaffing scenarios, both of which can have detrimental effects on patient outcomes. Understaffing can lead to delayed responses to patient needs, increased stress among staff, and ultimately, a decline in the quality of care provided. Conversely, overstaffing can lead to unnecessary operational costs, which might divert resources from other critical areas.
Linking Time Management to Healthcare Outcomes
Time management in healthcare is intrinsically linked to overall healthcare outcomes. Effective scheduling and attendance tracking ensure that healthcare professionals are not overworked, which reduces the risk of burnout and errors. Studies have shown that healthcare providers who work excessive hours or irregular shifts are more prone to making mistakes that can adversely affect patient care. For instance, a 2019 study published in the Journal of General Internal Medicine found that medical errors were three times more likely to occur when healthcare professionals worked shifts longer than 12 hours compared to standard 8-hour shifts.
Furthermore, efficient time and attendance management allows for better coordination among multidisciplinary teams, ensuring that patient care plans are executed smoothly and promptly. This level of coordination is particularly crucial in acute care settings, where timely interventions can significantly improve patient outcomes.
Nurses & Long Hours Statistics
| Statistic | Detail |
|---|---|
| Patient Satisfaction and Nurse Shift Length | Shifts greater than 13 hours linked to patient dissatisfaction due to poor communication, uncontrolled pain, delayed help, and lower hospital recommendations. |
| Nurse Burnout and Job Dissatisfaction | Nurses working shifts greater than 13 hours had over double the risk for burnout and job dissatisfaction. |
| Error Risk with Long Shifts | Nurses had over 3 times the odds of making an error when working 12 or more hours compared to 8.5-hour shifts. |
| Critical Care Nursing Shift Length | Risk for patient care errors almost doubled and struggling to stay awake at work increased by 50% when shifts lasted longer than 12.5 hours. |
| Patient Mortality and Nurse Work Hours | Hospitals with higher patient mortality rates had higher rates of nurses working long hours, lacking time away from work, working while sick, and having higher weekly work hour burdens. |
| Weekly Work Hours and Adverse Outcomes | Working more than 40 hours per week was associated with increased risk for adverse patient outcomes, including errors and near misses, injury from falls, and nosocomial infections. |
| Institute of Medicine Recommendations | Recommended limiting nurse work hours to 60 hours or less in a 7-day period and no more than 12 hours in a 24-hour period. |
| Systematic Review Findings | Working more than 40 hours a week linked to adverse patient and nurse outcomes. |
| Penalties for Fatigue-Related Errors | Employers and workers have been penalized when a fatigue-related error led to a person’s death. |
Data Retrieved From: https://www.cdc.gov/niosh/work-hour-training-for-nurses/longhours/mod3/10.html
Medical Error Reduction & Prevention Statistics
| Statistic | Detail |
|---|---|
| Leading Cause of Death | Medical errors are the third leading cause of death in the US. |
| Preventable Harm in Hospitals | Approximately 400,000 hospitalized patients experience preventable harm each year. |
| Annual Patient Deaths | Over 200,000 patient deaths annually are due to preventable medical errors. |
| Cost of Adverse Events | Adverse events cost the healthcare system $20 billion each year. |
| Cost of Hospital-Acquired Infections | Healthcare costs for hospital-acquired infections range from $35.7 to $45 billion annually. |
| Types of Medical Errors |
|
| Psychological Impact on Healthcare Professionals |
Healthcare professionals may experience:
|
| Impact of Medical Errors |
Medical errors impact:
|
| Strategies to Reduce Medical Errors |
Strategies include:
|
Data Retrieved From: https://www.ncbi.nlm.nih.gov/books/NBK499956/
Incorporating Statistics to Emphasize Points
The importance of time and attendance management is further highlighted by statistics on staff turnover rates and their impact on patient care. According to the 2024 National Healthcare Retention & RN Staffing Report, the average turnover rate for registered nurses in the United States was 18.4%. High turnover rates not only increase recruitment and training costs but also disrupt continuity of care, leading to poorer patient outcomes.
Moreover, a study conducted by the American Nurses Association revealed that hospitals with lower staff turnover rates and better-managed schedules reported a 15% improvement in patient satisfaction scores. This correlation underscores the importance of retaining experienced staff through effective time and attendance management, as it contributes to higher quality care and better patient experiences.
Another critical statistic is related to absenteeism. The U.S. Bureau of Labor Statistics reported that in 2023, the absenteeism rate in the healthcare sector was 3.8%; higher than the national average across almost all industries. Effective time and attendance systems can help reduce absenteeism by providing insights into attendance patterns, allowing management to address issues proactively.
2024 NSI National Health Care Retention & RN Staffing Report Statistics Table
| Metric | Value |
|---|---|
| Average Staff RN Turnover Rate | 18.4% |
| Average Staff RN Turnover Rate (Full and Part Time) | 15.0% |
| 1st Year Employee Turnover Rate | 30.2% |
| 1st Year RN Turnover Rate | 23.8% |
| Cost of Each RN Turnover | $56,277 |
| Annual Average Hospital Cost of RN Turnover | $4.82 million |
| Average Annual Cost/Savings per 1% Change in RN Turnover | $262,544 |
| Percent of Involuntary Turnover | 4.6% |
| 2024 Hospital Retention Goal | 3.0% |
| Average Hospital RN Vacancy Rate | 9.9% |
| Average RN Time-to-Fill | 86 days |
| Percent Anticipating to Increase Workforce | 68.9% |
| Percent Anticipating to Increase RN Workforce | 71.1% |
| Percent Anticipating to Increase Recruitment Budget | 36.3% |
| Percent Anticipating to Increase Recruitment Staff | 23.8% |
| HR to Employee Ratio (per 100 employees) | 0.87 |
| Recruitment to Employee Ratio (per 100 employees) | 0.28 |
| Percent Anticipating to Decrease Travel/Agency Usage | 80.0% |
‘Pro-Tip’
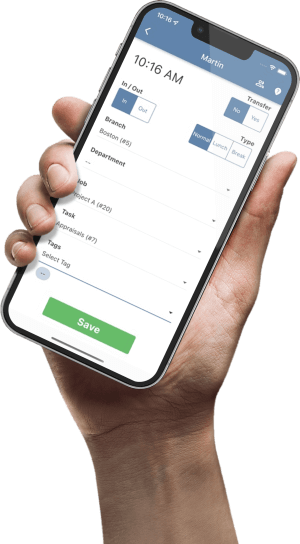
Utilize Mobile Access for Flexibility: Enable healthcare staff to clock in and out using TimeTrex’s mobile app, which supports GPS tracking and geofencing. This is particularly useful for home healthcare providers and staff who work across multiple locations, ensuring accurate time tracking regardless of their location.
Common Challenges in Healthcare Time and Attendance
Typical Issues in Scheduling, Shift Swapping, and Overtime Management
Healthcare facilities operate around the clock, requiring meticulous scheduling to ensure that adequate staff is available at all times. However, scheduling in healthcare is fraught with challenges, including the need to accommodate diverse shift patterns, handle last-minute shift changes, and manage overtime efficiently.
Scheduling: Creating and maintaining schedules that meet the needs of both patients and staff can be a logistical nightmare. Balancing shift preferences, ensuring compliance with labor laws, and avoiding scheduling conflicts require sophisticated systems and significant administrative effort. For example, a large hospital might need to schedule hundreds of nurses across various departments, each with different skill sets and availability.
Shift Swapping: Shift swapping is a common occurrence in healthcare due to the unpredictable nature of personal emergencies and the demanding nature of the job. However, managing these swaps manually can lead to confusion, errors, and gaps in coverage. A nurse might need to swap a shift last minute due to a family emergency, but without a streamlined system, this can result in understaffing if the swap isn’t recorded correctly.
Overtime Management: Overtime is another significant challenge. While sometimes unavoidable, excessive overtime can lead to staff burnout, increased error rates, and higher operational costs. For instance, a study by the University of California found that nurses working shifts longer than 12 hours were more likely to experience burnout and job dissatisfaction, which can negatively impact patient care.
Implications of Understaffing and Overstaffing
Understaffing: When a healthcare facility is understaffed, the quality of patient care suffers. Patients may experience longer wait times, reduced one-on-one time with healthcare providers, and a higher likelihood of medical errors. Understaffing also places tremendous stress on existing staff, leading to burnout and increased turnover rates. For example, during the COVID-19 pandemic, many hospitals faced severe understaffing, which compromised patient care and led to high levels of burnout among healthcare workers.
Overstaffing: On the flip side, overstaffing can be just as problematic, albeit in different ways. Overstaffing leads to unnecessary labor costs, which can strain the financial resources of healthcare facilities. This can result in reduced budgets for other critical areas such as medical equipment, patient care programs, and facility maintenance. An overstaffed unit might also experience lower staff morale, as employees may feel underutilized and disengaged.
Nurse Burnout Statistics
| Metric | Value |
|---|---|
| Nurses Experiencing Moderate Burnout | 54% |
| Nurses Experiencing High Burnout | 28% |
| Increase in Emotional Exhaustion Scores After 1 Year | 10% |
| Increase in Cynicism Scores After 1 Year | 19% |
| Organizational Turnover Due to Burnout (Increase per Unit on Emotional Exhaustion Scale) | 12% |
| Position Turnover Due to Burnout | Not a Factor |
| Burnout Prevalence in Nursing Workforce (US) | 19% to 43% |
| Average Nurse Exposure to Patient Deaths per Month | 0.477 |
| Average Nurse Exposure to Patient Deaths per Month (High Acuity Areas) | 1.5 |
| Nurse Resilience Score (2018) | 32.59 |
| Nurse Resilience Score (2019) | 31.83 |
| Annual Organizational Turnover Rate for Nurses | 8% |
| Annual Position Turnover Rate for Nurses | 8% |
| Nurse Burnout Due to Death Exposure (Increase per Death per Month) | 40% |
Data Retrieved From: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7532952/
‘Pro-Tip’
Automate Scheduling to Reduce Administrative Burden: Take advantage of TimeTrex’s automated scheduling capabilities to manage complex shift patterns and staff availability. Automated alerts for overtime, shift changes, and compliance issues help reduce scheduling errors and administrative workload.
Legal and Compliance Aspects
Relevant Labor Laws and Regulations
Healthcare facilities must navigate a complex web of labor laws and regulations to ensure compliance and avoid legal repercussions. Understanding and adhering to these laws is crucial for maintaining operational integrity and protecting both employees and patients.
Fair Labor Standards Act (FLSA): The FLSA sets the federal standards for minimum wage, overtime pay, recordkeeping, and youth employment. For healthcare facilities, this means ensuring that all non-exempt employees are paid at least the federal minimum wage and receive overtime pay at one and a half times their regular rate for any hours worked over 40 in a workweek. Accurate time and attendance records are essential to demonstrate compliance with these requirements.
Family and Medical Leave Act (FMLA): The FMLA entitles eligible employees to take unpaid, job-protected leave for specified family and medical reasons. Healthcare employers must accurately track employee hours and leave to ensure that eligible employees receive their entitled leave and that their positions are protected during their absence.
State-Specific Labor Laws: In addition to federal laws, healthcare facilities must comply with state-specific labor laws, which can vary significantly. For example, California has stringent overtime regulations that require daily overtime pay for hours worked over eight in a day and double-time pay for hours worked over twelve in a day. States like New York have specific requirements for meal and rest breaks. It is essential for healthcare facilities to stay informed about and comply with the specific labor laws in their state.
Occupational Safety and Health Administration (OSHA): OSHA regulations ensure safe and healthful working conditions. Accurate time and attendance tracking can help healthcare facilities identify patterns of excessive work hours that may contribute to fatigue and increase the risk of workplace injuries, thus aiding in compliance with OSHA standards.
Consequences of Non-Compliance
Failing to comply with labor laws and regulations can have severe consequences for healthcare facilities, ranging from financial penalties to reputational damage.
Financial Penalties: Non-compliance with labor laws such as the FLSA can result in substantial fines and penalties. For instance, violations of minimum wage and overtime provisions can lead to back pay awards and damages. In severe cases, employers may face civil money penalties of up to $1000 per violation for repeated or willful violations of the FLSA.
Litigation Costs: Non-compliance can also lead to costly lawsuits. Employees may file claims for unpaid wages, overtime, or wrongful termination. Legal battles not only drain financial resources but also divert attention from core healthcare operations.
Reputational Damage: Healthcare facilities found to be in violation of labor laws can suffer significant reputational damage. Negative publicity can erode trust among patients, employees, and the community, making it more challenging to attract and retain both staff and patients.
Operational Disruptions: Non-compliance can lead to increased scrutiny from regulatory bodies, resulting in audits and inspections that disrupt daily operations. This added scrutiny can strain administrative resources and impact the facility’s ability to deliver quality care.
‘Pro-Tip’
Ensure Compliance with Labor Laws: Leverage TimeTrex’s compliance management tools to automatically track and report on labor law requirements, such as overtime, meal breaks, and state-specific regulations. This helps healthcare facilities avoid costly legal penalties and maintain compliance.
Technological Solutions for Time and Attendance
Modern Software Solutions Tailored for Healthcare
In the digital age, healthcare facilities can leverage advanced technological solutions to address the complex challenges of time and attendance management. These solutions are designed to enhance accuracy, improve compliance, and boost overall efficiency. Here are some of the most impactful technologies tailored for the healthcare sector:
Biometric Time Clocks: Biometric time clocks use fingerprint, facial recognition, or iris scanning technology to ensure that time and attendance data is accurate and secure. These systems eliminate the possibility of “buddy punching,” where one employee clocks in or out for another. Biometric clocks also streamline the process of clocking in and out, reducing the time employees spend on administrative tasks.
Mobile Apps: Mobile time and attendance apps allow healthcare staff to clock in and out from their smartphones or tablets. These apps are particularly useful for home healthcare providers and other mobile healthcare workers who are not always on-site. Features such as GPS tracking and geofencing ensure that employees are clocking in and out from authorized locations, adding an extra layer of accuracy and security.
Automated Scheduling Software: Automated scheduling solutions help healthcare facilities manage complex shift patterns and staffing requirements. These systems can generate optimized schedules based on employee availability, qualifications, and labor laws. Automated alerts for shift changes, overtime, and compliance issues help administrators stay ahead of potential problems.
Cloud-Based Systems: Cloud-based time and attendance systems offer flexibility and scalability, making it easy for healthcare facilities to manage their workforce from anywhere. These systems provide real-time access to attendance data, allowing managers to make informed decisions quickly. Integration with other HR and payroll systems ensures seamless data flow and reduces administrative burden.
Benefits of Integrating Such Technologies
Accuracy: Modern time and attendance technologies greatly enhance the accuracy of attendance records. Biometric systems, for example, ensure that the data collected is precise and tamper-proof. This accuracy helps prevent payroll discrepancies and ensures that employees are paid correctly for the hours they work.
Compliance: Integrating advanced time and attendance systems helps healthcare facilities stay compliant with labor laws and regulations. Automated tracking and reporting features ensure that all legal requirements, such as overtime and meal break rules, are met consistently. These systems can generate compliance reports, making it easier to demonstrate adherence during audits and inspections.
Efficiency: The automation of time and attendance processes significantly reduces the administrative workload. Automated scheduling, real-time attendance tracking, and integration with payroll systems streamline operations and free up time for managers to focus on more strategic tasks.
‘Pro-Tip’
Integrate with Payroll and HR Systems: Integrate TimeTrex with your existing payroll and HR systems to streamline data flow and reduce manual data entry. This ensures accurate and timely payroll processing, minimizes errors, and saves administrative time.
How to Choose the Right Time and Attendance System
Factors to Consider
Selecting the appropriate time and attendance system for a healthcare facility requires careful consideration of several key factors to ensure it meets the specific needs of the organization and its workforce.
Integration with Existing Systems:
One of the most critical factors to consider is how well the new time and attendance system will integrate with existing systems, such as payroll, HR, and scheduling software. Seamless integration ensures that data flows smoothly between systems, reducing the need for manual data entry and minimizing the risk of errors. For instance, a system that automatically transfers attendance data to the payroll software can streamline the payroll process and ensure accurate and timely payments.
Scalability:
Healthcare facilities can range from small clinics to large hospitals, and their needs may evolve over time. It’s essential to choose a time and attendance system that can scale with the organization. A scalable system can accommodate growth in the number of employees, new locations, or additional departments without requiring a complete overhaul. This flexibility is crucial for long-term sustainability and cost-effectiveness.
User-Friendliness:
A user-friendly interface is vital for ensuring that all staff members, from administrators to frontline healthcare workers, can easily navigate the system. The system should have intuitive features that make clocking in and out, requesting leave, and managing schedules straightforward. A complicated or cumbersome system can lead to frustration, errors, and lower adoption rates among staff.
Compliance Features:
Given the stringent labor laws and regulations in the healthcare sector, it’s important to select a system that includes robust compliance features. This includes automated alerts for overtime, meal breaks, and other regulatory requirements. A system that generates detailed compliance reports can help healthcare facilities demonstrate adherence to labor laws and avoid potential legal issues.
Importance of Support and Training for Staff
Comprehensive Training Programs:
Implementing a new time and attendance system requires thorough training to ensure that all staff members are comfortable and proficient in using the new technology. Training should be tailored to different user groups within the organization, including administrators, managers, and frontline staff. This ensures that everyone understands how to use the system effectively and can leverage its features to their full potential. Offering various training formats, such as in-person sessions, webinars, and online tutorials, can accommodate different learning preferences and schedules.
Ongoing Support:
Even after the initial implementation and training, ongoing support is crucial for addressing any issues that arise and ensuring the system continues to operate smoothly. Look for a vendor that offers robust customer support, including helpdesk services, regular system updates, and proactive maintenance. Having access to reliable support can prevent disruptions and keep the system running efficiently, minimizing downtime and ensuring continuous compliance.
Feedback Mechanisms:
Implementing a new system is an ongoing process that benefits from continuous improvement. Establishing feedback mechanisms allows staff to provide input on their experiences with the system. This feedback can be invaluable for identifying areas where additional training might be needed or where the system could be optimized to better meet the needs of the organization. Regularly soliciting and acting on feedback helps ensure that the system evolves in a way that supports the workforce and enhances overall efficiency.
‘Pro-Tip’
Track Overtime and Prevent Burnout: Monitor overtime and manage workloads effectively with TimeTrex’s overtime tracking features. By keeping a close eye on overtime, healthcare facilities can prevent staff burnout and ensure a healthier work environment.
Future Trends in Time and Attendance Management
Upcoming Innovations
The landscape of time and attendance management is rapidly evolving, driven by advancements in technology. Several emerging trends promise to further revolutionize how healthcare facilities manage their workforce, leading to enhanced efficiency, accuracy, and compliance. Here are some key innovations to watch:
Artificial Intelligence (AI) and Machine Learning:
AI and machine learning are set to play a transformative role in time and attendance management. These technologies can analyze vast amounts of data to identify patterns and predict staffing needs with remarkable accuracy. For instance, machine learning algorithms can forecast peak times when additional staff is required, based on historical data and real-time variables such as patient admissions and seasonal trends. AI can also automate complex scheduling tasks, optimizing shift patterns to balance workloads and reduce overtime.
Internet of Things (IoT):
IoT devices are increasingly being integrated into time and attendance systems. Wearable devices such as smart badges and wristbands can track employee movements and automatically record attendance when staff enter and exit designated areas. These devices can also monitor employee health metrics, such as fatigue levels, to ensure that healthcare workers are not overworked, thereby enhancing both employee well-being and patient safety. Additionally, IoT-enabled sensors can provide real-time data on occupancy levels in different areas of a facility, helping managers make informed decisions about staffing allocation.
Blockchain Technology:
Blockchain technology offers a secure and transparent way to record and verify time and attendance data. By creating immutable records, blockchain ensures that attendance data cannot be tampered with, enhancing trust and compliance. This technology can also facilitate secure and efficient sharing of attendance data between different departments and external agencies, such as labor regulators, without compromising privacy.
Voice and Facial Recognition:
Advanced biometric systems are incorporating voice and facial recognition technologies to enhance security and convenience. These systems can quickly and accurately verify employee identities, reducing the time spent on clocking in and out. For healthcare facilities, this means that staff can spend more time on patient care and less time on administrative tasks.
Predictive Analytics:
Predictive analytics tools use historical data to anticipate future staffing needs and potential issues. For example, they can predict which employees are most likely to call in sick based on past behavior and external factors such as flu season. This allows managers to proactively arrange for backup staff, ensuring that patient care is not compromised.
How These Changes Could Reshape Healthcare Administration
Enhanced Workforce Efficiency:
The integration of AI, machine learning, and IoT can significantly enhance workforce efficiency in healthcare facilities. Predictive analytics can optimize staffing levels, ensuring that the right number of healthcare professionals are available when needed, reducing both understaffing and overstaffing. Automated scheduling and real-time attendance tracking can free up administrative staff from routine tasks, allowing them to focus on more strategic activities.
Improved Compliance and Security:
Blockchain and advanced biometric systems can improve compliance with labor laws and regulations by ensuring accurate and tamper-proof attendance records. This not only helps healthcare facilities avoid legal issues but also builds trust with employees by ensuring fair and transparent timekeeping practices. Enhanced security measures provided by biometric authentication can also protect sensitive employee data from breaches.
Better Employee Well-being:
Wearable IoT devices and AI-driven fatigue monitoring can help healthcare facilities monitor the well-being of their staff in real-time. By identifying signs of fatigue or stress early, these technologies enable managers to take proactive measures, such as redistributing workloads or providing additional support, to prevent burnout. This leads to a healthier, more satisfied workforce, which in turn can improve patient care and reduce turnover rates.
Data-Driven Decision Making:
The ability to collect and analyze large amounts of data from various sources will empower healthcare administrators to make more informed decisions. Predictive analytics and machine learning can provide insights into workforce trends, helping managers develop more effective staffing strategies and identify potential issues before they become problems. This data-driven approach can lead to more efficient operations and better resource allocation.
Enhanced Patient Care:
Ultimately, the goal of any improvement in healthcare administration is to enhance patient care. By optimizing staffing levels, reducing administrative burdens, and ensuring that healthcare workers are well-supported and not overworked, these technological advancements can lead to better patient outcomes. More efficient time and attendance management means that healthcare providers can spend more time with patients, leading to higher quality care and improved patient satisfaction.
‘Pro-Tip’
Enhance Employee Engagement with Self-Service Options: Empower healthcare staff by providing them with self-service access through TimeTrex. Employees can view their schedules, request time off, and swap shifts easily, improving engagement and satisfaction.
Frequently Asked Questions (FAQ)
How can time and attendance systems improve patient care?
Time and attendance systems ensure that healthcare facilities are adequately staffed at all times, reducing the risk of understaffing that can lead to delayed patient care. Accurate tracking and scheduling allow for better allocation of resources, ensuring that patients receive timely and appropriate care. Additionally, these systems help prevent staff burnout by distributing workloads more evenly, resulting in better overall patient care.
What are the common challenges in healthcare time tracking?
Healthcare time tracking faces challenges such as managing complex schedules, handling shift swaps, ensuring compliance with labor laws, and preventing payroll discrepancies. Other issues include dealing with high turnover rates, accommodating various staff roles, and maintaining accurate records in a 24/7 operation.
What features should a healthcare time and attendance system have?
A comprehensive healthcare time and attendance system should include features such as biometric authentication, mobile clock-in/clock-out, automated scheduling, real-time attendance tracking, integration with payroll and HR systems, compliance management tools, and robust reporting capabilities.
How do biometric systems enhance security in healthcare settings?
Biometric systems use unique physical characteristics such as fingerprints, facial recognition, or iris scans to verify employee identities. This ensures that attendance records are accurate and prevents “buddy punching” (when one employee clocks in or out for another). Biometric systems also enhance security by protecting sensitive employee data and reducing the risk of time theft.
What are the future trends in healthcare time and attendance technology?
Future trends include the integration of AI and machine learning for predictive scheduling and workload management, IoT devices for real-time tracking and monitoring, blockchain technology for secure and tamper-proof record-keeping, and advanced biometric systems incorporating voice and facial recognition. These innovations aim to improve efficiency, accuracy, compliance, and overall employee well-being.
How can a healthcare facility choose the right time and attendance system?
Healthcare facilities should consider factors such as integration with existing systems, scalability, user-friendliness, compliance features, and the quality of support and training provided by the vendor. Evaluating these factors ensures that the chosen system meets the specific needs of the facility and its workforce.
What are the consequences of non-compliance with labor laws in healthcare?
Non-compliance with labor laws can result in financial penalties, costly lawsuits, reputational damage, and operational disruptions. For example, violations of the Fair Labor Standards Act (FLSA) can lead to back pay awards, damages, and civil money penalties. Ensuring compliance helps avoid these negative outcomes and maintains trust with employees and regulatory bodies.
How do automated scheduling systems benefit healthcare facilities?
Automated scheduling systems help healthcare facilities manage complex shift patterns, optimize staffing levels, reduce scheduling errors, and ensure compliance with labor laws. These systems can generate efficient schedules based on employee availability and qualifications, send automated alerts for shift changes, and provide real-time data for better decision-making.
Why is support and training important when implementing a new time and attendance system?
Support and training are crucial to ensure that all staff members are comfortable and proficient in using the new system. Comprehensive training programs tailored to different user groups and ongoing support help address any issues that arise, ensure smooth operation, and maximize the system’s benefits. Proper training and support lead to higher adoption rates and more effective use of the system.
How can predictive analytics improve time and attendance management in healthcare?
Predictive analytics use historical data to forecast future staffing needs, identify potential issues, and optimize schedules. By predicting peak times, likely sick days, and staffing requirements, healthcare facilities can proactively arrange for backup staff, prevent understaffing, and ensure that patient care is not compromised. This data-driven approach enhances operational efficiency and reduces the risk of errors.
What are the benefits of mobile time and attendance apps for healthcare workers?
Mobile time and attendance apps offer flexibility for healthcare workers, allowing them to clock in and out from their smartphones or tablets, whether they are on-site or working remotely. Features like GPS tracking and geofencing ensure accurate location-based clocking, while mobile access to schedules and shift swaps improves convenience and efficiency for staff.
Disclaimer: The content provided on this webpage is for informational purposes only and is not intended to be a substitute for professional advice. While we strive to ensure the accuracy and timeliness of the information presented here, the details may change over time or vary in different jurisdictions. Therefore, we do not guarantee the completeness, reliability, or absolute accuracy of this information. The information on this page should not be used as a basis for making legal, financial, or any other key decisions. We strongly advise consulting with a qualified professional or expert in the relevant field for specific advice, guidance, or services. By using this webpage, you acknowledge that the information is offered “as is” and that we are not liable for any errors, omissions, or inaccuracies in the content, nor for any actions taken based on the information provided. We shall not be held liable for any direct, indirect, incidental, consequential, or punitive damages arising out of your access to, use of, or reliance on any content on this page.
About The Author

Roger Wood
With a Baccalaureate of Science and advanced studies in business, Roger has successfully managed businesses across five continents. His extensive global experience and strategic insights contribute significantly to the success of TimeTrex. His expertise and dedication ensure we deliver top-notch solutions to our clients around the world.
Time To Clock-In
Start your 30-day free trial!
Experience the Ultimate Workforce Solution and Revolutionize Your Business Today
- Eliminate Errors
- Simple & Easy To Use
- Real-time Reporting
Saving businesses time and money through better workforce management since 2003.
Copyright © 2025 TimeTrex. All Rights Reserved.